INTRODUCTION
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired, clonal, nonmalignant hematologic disease characterized by complement-mediated red blood cell hemolysis. The current standard of care for patients with PNH is C5 inhibition. Anemia persists in up to ~70% of patients receiving eculizumab and is attributed to persistent intravascular hemolysis (IVH) and mostly to C3-mediated extravascular hemolysis (EVH). Pegcetacoplan is a pegylated pentadecapeptide C3 inhibitor targeting proximal complement to control both IVH and EVH. PEGASUS is a phase 3, open-label, active-comparator controlled study of efficacy and safety of pegcetacoplan versus eculizumab. This post hoc analysis of data from PEGASUS categorized the clinical response to pegcetacoplan or ECU in patients with PNH and hemoglobin <10.5 g/dL (despite stable ECU for ≥3 months).
METHODS
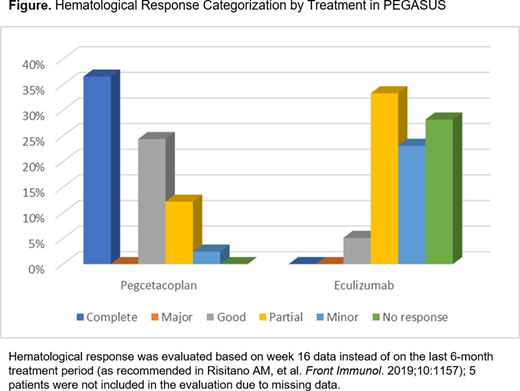
Hematologic response to treatment was categorized (per Risitano AM, et al. Front Immunol. 2019;10:1157) as complete, major, good, partial, minor, or no response, using number of packed red blood cell transfusions required, hemoglobin level, lactate dehydrogenase (LDH) level, and absolute reticulocyte count (ARC). Complete response: no transfusions required, stable hemoglobin in the normal range, and no evidence of hemolysis (ie, LDH ≤1.5× upper limit of normal, ARC ≤150,000/µL). Major response: no transfusion, normal hemoglobin, but with evidence of hemolysis (LDH >1.5× upper limit of normal and/or ARC >150,000/µL). Good response: no transfusion, but with chronic mild anemia or evidence of hemolysis. Partial response: chronic moderate anemia and/or occasional transfusions (<3 units/6 months). Minor response: regular transfusions required (3-6 units/6 months). No response: regular and frequent transfusions required (>6 units/6 months). Nine patients (6 from the pegcetacoplan arm and 3 from the eculizumab arm) did not readily fit within the existing criteria due to the availability of data at week 16. Although these 9 patients were manually categorized identically by the lead and senior author in a blinded, independent manner, they were not included among these data.
RESULTS
The intention-to-treat population was comprised of 41 patients randomized to pegcetacoplan and 39 patients randomized to eculizumab. Four patients in the pegcetacoplan arm and 1 patient in the eculizumab arm were not evaluable for analysis due to incomplete data at week 16. Altogether, 61.0% of patients (25/41) in the pegcetacoplan arm have achieved at least a good hematological response, in contrast to 5.1% (2/39) of the eculizumab arm. At week 16, the distribution of response categories was as follows (Figure): in the pegcetacoplan arm and eculizumab arm, respectively, complete responses were 36.6% and 0%, good responses were 24.4% and 5.1%, partial responses were 12.2% and 33.3%, minor responses were 2.4% and 23.1%, and no responses were 0% and 28.2%. The addition of the 9 manually categorized patients did not significantly alter the proportions reported here. Among the factors that may contribute to heterogeneity of hematologic response to treatment are impaired bone marrow function, residual IVH, and residual C3-mediated EVH. Bone marrow failure was ruled out, and no difference in LDH was observed, suggesting that the major factor accounting for the difference between the 2 arms was the prevention of C3-mediated EVH (as confirmed by reduction of C3-opsonization of PNH red blood cells).
CONCLUSION
In PEGASUS, treatment with pegcetacoplan resulted in a greater proportion of patients with better hematological responses compared to eculizumab. These results further support the concept that proximal complement inhibition, by preventing EVH in addition to controlling IVH, leads to clinical and hematological improvement in the treatment of PNH.
Risitano:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Alnylam: Research Funding; Alexion: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Samsung: Membership on an entity's Board of Directors or advisory committees; Amyndas: Consultancy; RA pharma: Research Funding; Biocryst: Membership on an entity's Board of Directors or advisory committees; Achillion: Membership on an entity's Board of Directors or advisory committees; Jazz: Speakers Bureau; Roche: Membership on an entity's Board of Directors or advisory committees; Pfizer: Speakers Bureau; Apellis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Weitz:Alexion: Consultancy, Honoraria, Speakers Bureau; Apellis: Consultancy, Honoraria. de Castro:Novartis: Honoraria, Other: Steering committee; Alexion: Honoraria, Research Funding; Biocryst: Honoraria, Other: Data monitoring committee; Apellis: Consultancy, Honoraria, Research Funding. Kiladjian:AbbVie: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees; AOP Orphan: Membership on an entity's Board of Directors or advisory committees. Griffin:Biocryst: Membership on an entity's Board of Directors or advisory committees; Alexion Pharmaceuticals: Honoraria, Other: Conference Support. Hamdani:Apellis: Current Employment, Current equity holder in publicly-traded company. Ajayi:Apellis Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Baver:Apellis: Current Employment, Current equity holder in publicly-traded company. Peffault De Latour:Novartis: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Amgen: Research Funding; Alexion Pharmaceuticals Inc.: Consultancy, Honoraria, Research Funding.
Pegcetacoplan is an investigational drug for the treatment of paroxysmal nocturnal hemoglobinuria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal